Blog
Useful and free info on dental implants, cosmetic dentistry, family dentistry, and more. All posts written by our doctors, not AI or some outside marketing firm. If you are in Campton Hills, St Charles, Geneva, Batavia, Elburn, Elgin, or anywhere in Kane County, these posts will be helpful!
Do Wisdom Teeth Really Need to be Extracted?
Are you wondering whether wisdom teeth are really a problem? Or does your child really need them removed? Below are some things to consider and the risks you should know about.
Why Wisdom Teeth Can Be a Problem
While some wisdom teeth grow in without causing issues, others create complications that make you wonder why people have them in the first place. Here are a few common problems that can arise:
Infection: When wisdom teeth only partially emerge, they leave behind gum pockets that trap bacteria, leading to painful infections like pericoronitis. A study in the International Journal of Environmental Research and Public Health found that pericoronitis is one of the most common complications of retained wisdom teeth.
Gum Disease: Wisdom teeth are often difficult to clean, making them a breeding ground for bacteria that contribute to gum disease. Research in the Journal of Clinical Periodontology shows that infections around wisdom teeth can increase the risk of periodontal disease in neighboring teeth.
Tooth Decay: Because wisdom teeth are so far back in the mouth, they can be tricky to reach with a toothbrush or floss. According to the Journal of the American Dental Association, wisdom teeth are significantly more prone to cavities than other molars.
Crowding & Shifting: Even if your wisdom teeth aren’t painful, they can push against your other teeth, potentially undoing years of orthodontic work.
Cysts & Jaw Damage: Impacted wisdom teeth can sometimes form cysts, which may damage the surrounding bone and even require more extensive treatment.
Because younger patients heal faster and experience fewer complications, wisdom teeth are often removed in the late teens or early 20s.
Why don’t wisdom teeth fit in our mouth?
You may be asking why our ancestors’ wisdom teeth fit in their mouth, but ours don’t. The book “Jaws” has a very interesting anthropological take on the subject. It closely aligns with our thinking at Teuscher Legacy Dental, and is highly recommended reading from Dr Andrew Huberman, Jared Diamond, Robert Sapolsky, and others.
Why Choose Teuscher Legacy Dental for Wisdom Teeth Removal?
At Teuscher Legacy Dental, we make the wisdom teeth removal process as seamless and stress-free as possible. Here’s what sets us apart:
Patient-Centered Comfort: From thorough consultations to post-op care, we prioritize your comfort at every step.
Personalized Attention: Because we know your dental history, we can make the best recommendations for your individual case and offer continuity of care.
Convenient In-Office Extractions: No need to travel to a specialist— Dr Brayden Teuscher performs most wisdom teeth removals right here in our St. Charles office.
Affordable Care: Our fees are often lower than those of oral surgeons, without sacrificing quality.
Sedation Options: We offer safe, effective oral sedation to help ease any anxiety you may have during the procedure.
When Should You See an Oral Surgeon?
While most wisdom teeth extractions can be performed in our office, there are certain cases where we may recommend an oral surgeon:
If IV sedation is necessary for a deeper level of anesthesia
If the teeth are severely impacted or in a particularly difficult position
If there is a high risk of nerve involvement or other surgical complexities
If we determine that an oral surgeon is the best option for you, we’ll guide you through the referral process and ensure you receive the best care possible.
Wisdom from Master Yoda
“Wisdom teeth- misnamed they are. Pain they bring. Wisdom, they do not!”
What to Expect When Having Wisdom Teeth Removed
We understand that any dental procedure can feel overwhelming, but we’ll be with you every step of the way. Here’s how the process works:
Step 1: Consultation & X-Rays
During your initial visit, we’ll take X-rays to assess the position of your wisdom teeth and determine whether removal is the best course of action. We’ll also discuss your sedation options to ensure a smooth, comfortable experience.
Step 2: The Procedure
On the day of your extraction, you’ll be in good hands. We’ll carefully remove the teeth while keeping you as comfortable as possible. Most procedures take less than an hour.
Step 3: Recovery & Healing
Every patient is different, but most people recover within a few days. We’ll provide detailed aftercare instructions, including tips on managing swelling, what to eat, and how to care for the extraction sites. We’re always just a phone call or text away if you have any concerns.
Are Your Wisdom Teeth Causing You Pain?
If you’re experiencing discomfort, swelling, or just want to know whether your wisdom teeth should stay or go, we’re here to help. At Teuscher Legacy Dental, we’ve helped countless patients in St. Charles, Elburn, Geneva, and the surrounding areas navigate wisdom teeth removal with confidence. Schedule a consultation today, and let’s make a plan that’s right for you!
📍 Location: 40W131 Campton Crossings Drive, St. Charles, IL 60175
📞 Phone: 630-762-0000
🌐 Website: TeuscherDental.com
Sources:
A. Alqahtani et al., "Pericoronitis and Its Management in Young Adults," International Journal of Environmental Research and Public Health, 2021.
S. D. White & M. L. Pharoah, "Oral Health Implications of Wisdom Teeth," Journal of Clinical Periodontology, 2012.
D. L. Weyant, & A. L. Jay, “Impacted Wisdom Teeth and Caries Risk: A Review,” Journal of the American Dental Association, 2013.
Fluoride and Your Family's Health: A Father’s Reflections
I’m a dentist, and my kids don’t use fluoride toothpaste.
Is that because I think fluoride is ineffective? No! In fact, it is perhaps the easiest, most cost effective prevention strategy for tooth decay.
So why don’t my kids use it? The answer is not as black and white as many assume. There is a lot of science to support fluoride use. But there’s also a strong rationale against. Below are some thoughts for and against fluoride, and how I as a dentist and father recommend you think about it for your family. I’ve also listed questions you should ask yourself to decide whether fluoride application is best for your family!
*note: I am not trying to choose any political side here. I am intentionally not commenting on matters of public policy. This is about YOU and thinking through what’s best for YOUR FAMILY.*
In support of fluoride:
Fluoride is a great way to strengthen teeth and prevent tooth decay. Numerous studies show this. But, as with any health topic, there's more to consider. Let’s explore the health implications of fluoride use both topically (through toothpaste or treatments applied to teeth) and systemically (through drinking water or supplements) so you can make an informed choice about what’s best for your family’s dental care.
Benefits of Topical Fluoride
Topical just means something that is set on the teeth. This is found in toothpastes, mouth rinses, and professional treatments. It directly strengthens the outer enamel of teeth, and as Dr Andrew Huberman and I have said, can even reverse early stages of decay. One particular study showed fluoride in toothpaste can reduce cavities by 26% (1).
The CDC says tooth decay is the most common disease of childhood in the US, so fluoride as a cavity reduction strategy is a huge deal! The CDC advises that when children brush daily with a fluoride toothpaste or get topical application at their dental hygiene visits, they’re getting a powerful shield against cavities (2).
Benefits of Ingested Fluoride (Fluoridated tap water)
When fluoride is ingested, through drinking water or supplements, it enters the bloodstream and becomes part of the developing teeth under the gums. This process can make teeth more resistant to decay even before they appear. This is particularly helpful in remote areas where fluoride sources or professional dental care may be more limited (3). Teeth aside, there aren’t other known benefits to ingesting fluoride.
Fluoride Saves Money
Research highlights that for every dollar spent on fluoride in drinking water, families save on future dental care costs due to reduced need for treatments (4). Actually, this exact same argument shows that getting regular dental cleanings saves money on healthcare costs. For families needing an easy, inexpensive, and straightforward way of cavity prevention, fluoride in drinking water could be a convenient, hands-off approach.
Fluoride Risks
Considerations of Ingested Fluoride
One concern over fluoride ingestion from tap water is that people who need to drink more water may be over-exposed to fluoride (5). While ingested fluoride does have established dental benefit, at high levels it is clearly toxic. Mild effects of too much fluoride consumption are dental fluorosis and some bone density changes (6,7,8,9). The bone density changes can be dangerous for some individuals. And more concerningly, very high levels of fluoride consumption have been linked to lower IQ, especially when consumed during pregnancy (10,11).
Note that these studies refer to ingesting fluoride (i.e., eating fluoride). These studies are NOT talking about toothpaste or topical fluoride application at a dental visit.
Considerations of Fluoride Toothpastes
While fluoride toothpaste is safe when used correctly, it can be tricky for young kids. Any parent of young kids knows they will eat the toothpaste! The amount they are ingesting in that case is likely so small as to not be of any concern, but for that reason, the American Dental Association (ADA) suggests a pea-sized amount of toothpaste for children ages 3-6, while those under 3 should use a “tiny smear”. This way, if they eat it, they wont actually take in much fluoride.
Eventually kids are big enough to know not to eat the toothpaste. They may still accidentally swallow some after brushing, but the fluoride ingestion will be negligible. With appropriate supervision, fluoride toothpaste should be a very effective, low-risk option for cavity prevention.
Balancing Topical and Ingested Fluoride for Overall Health
In summary, topical fluoride, such as toothpaste, offers highly controlled, direct benefits to enamel without entering the bloodstream. This can make it a low-risk, high-reward option. Ingested fluoride, through sources like drinking water, has similar benefits but more possible risk, particularly for parents mindful of dosage and other health factors.
Does Teuscher Legacy Dental recommend fluoride for their patients?
We sometimes recommend fluoride as a possible therapy. But not always!
For ingested fluoride, we are mostly talking about fluoridated tap water. If your family is happy drinking tap water, that’s great! I wouldn’t try and convince you otherwise. If the fluoride or other tap water content is concerning, a reverse osmosis water filter is a great way to purify. That’s what my family and I do.
For topical fluoride, we don’t have a universal recommendation. Our recommendations are always unique to each individual.
For example, if someone came to us at age 50 who had perfect teeth without any history of dental decay, in perfect systemic health, never ate sugar, and also never had used fluoride toothpaste and said they wanted to avoid fluoride, I’d encourage continuing to avoid it. They wouldn’t need the dental benefit. But if we saw a 17 year old with multiple existing cavities with a poor diet, acid reflux and poor homecare, we’d certainly offer fluoride as ONE OF the OPTIONS in a cavity prevention strategy. In this case, the possible risk of fluoride ingestion may be outweighed by its benefit in tooth disease prevention. We would never force it on anyone though.
We don’t ever use population level data or guidelines as the sole basis for your care recommendations. You are a unique individual with unique risk factors and preferences! Plus, cavity prevention is not as simple as fluoride or not.
If you aren’t sure whether fluoride is best for you and your family, talk to us. We definitely appreciate systemic toxicity concerns, and will work with you to help YOU DECIDE the best choice for your family.
In the mean time, here are some questions to help you decide whether you or someone in your family should use fluoride for tooth decay prevention:
-Do they have a previous history of cavities?
-Is there a family history of cavities?
-Do they have a diet rich in sugar or acid? (especially drinks)
-Is there already fluoride in the tap water?
-When was their last dental exam, and were there any areas of concern?
-Are they taking medications that cause dry mouth?
-Are they a mouth breather?
-Do they have a gut disease or other condition that would alter their mouth bacterial populations? (immunocompromised, gut dysbiosis, etc)
-Do they mouth breath chronically, or snore while asleep?
-Do they have acid reflux?
-Do they brush at least twice per day and floss once per day?
Let me know how we can help!
Dr Brayden Teuscher
Sources:
Marinho, V. C., Higgins, J. P., Logan, S., & Sheiham, A. (2003). Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews, 1. https://doi.org/10.1002/14651858.CD002279
Centers for Disease Control and Prevention (CDC). (2018). Community Water Fluoridation. Retrieved from https://www.cdc.gov/fluoridation/index.html
McDonagh, M. S., Whiting, P. F., Bradley, M., Cooper, J., Sutton, A. J., Chestnutt, I., ... & Kleijnen, J. (2000). A systematic review of public water fluoridation. BMJ, 321(7265), 855-859. https://doi.org/10.1136/bmj.321.7265.855
Griffin, S. O., Jones, K., & Tomar, S. L. (2001). An economic evaluation of community water fluoridation. Journal of Public Health Dentistry, 61(2), 78-86. https://doi.org/10.1111/j.1752-7325.2001.tb03371.
National Research Council. (2006). Fluoride in Drinking Water: A Scientific Review of EPA's Standards. National Academies Press.
Peckham, S., & Awofeso, N. (2014). Water fluoridation: a critical review of the physiological effects of ingested fluoride as a public health intervention. The Scientific World Journal, 2014, 293019. https://doi.org/10.1155/2014/293019
Susheela, A. K. (2001). Skeletal fluorosis: a review of the literature". Published in Environmental Health Perspectives.
Levy, S. M., & Leclerc, B. S. (2012). Fluoride intake of children: considerations for dental caries and dental fluorosis. Fluoride, 45(4), 243-248.
Dean, H. T. (2001). Classification of mottled enamel diagnosis. Public Health Reports, 65(17), 1019–1027.
Association between lifetime fluoride exposure and children's intelligence: A meta-analysis" by Choi, A. L., et al. (2012), published in Environmental Health Perspectives.
Green, R., Lanphear, B., Hornung, R., Flora, D., Martinez-Mier, E. A., Neufeld, R., ... & Till, C. (2019). Association between maternal fluoride exposure during pregnancy and IQ scores in offspring in Canada. JAMA Pediatrics, 173(10), 940-948. https://doi.org/10.1001/jamapediatrics.2019.1729
12. Images from my mom and Chat GPT!
Untethering the Secrets of Tongue and Lip Ties: A Three part letter to Moms
I had the medical knowledge. But when my son was diagnosed with a tongue and lip tie, the stakes got higher! Here is mother and father’s journey in navigating his tongue and lip ties.
Dear Moms,
I’m a father of 2 beautiful young boys, aged 2 and now 1 month! Being their Daddy is one of my greatest joys – and most profound responsibilities. Any parent wants the best for their children, but as any new parent realizes – there’s no 5 step parenting manual for perfect parenting! My wife and I are far from perfect parents (who can relate??!) but we are constantly seeking guidance and learning more. The weight of responsibility often feels heaviest with health decisions for our little ones, especially when there’s a level of uncertainty involved.
At our dental practice, we see a ton of kids and I’m constantly talking with parents about the growth of their kids’ jaws and tooth development. I’ve done extensive research on what factors influence this development and how jaw development affects their overall well-being. I felt very comfortable with my perspective on these issues. BUT when my second son was born with a tongue and lip tie, the stakes got higher! I had the knowledge, but still felt a protective father’s anxiety over how to best help my little guy. And my wife and I wanted to learn more.
Our family
As our family navigated this journey, we doubled down on researching tongue and lip ties from all perspectives. Ultimately we decided it was best for our son to get his tongue tie and lip tie released, but along the way we learned a lot and talked with many other parents who were going through the same dilemma. In this three part series I’m going to share the insights we gained, particularly from a holistic perspective, to help empower you to make informed decisions for your own little one.
Part 1 defines a tongue or lip tie and discusses the associated risks
Part 2 describes our emotional journey as parents, the consultations we had, and ultimately the procedure itself
Part 3 describes what happens after the frenectomy – home care and healing process
**Disclaimer – I will not be advocating that every frenum get released. That decision is always made after first considering all the risk factors unique to your own child, from a multidisciplinary perspective. Just because frenectomies were the choice we made does not mean that’s the best route for your own child. I just want to share our experience. I hope it helps you and your family!
Part 1: The Hidden Risks of Untreated Tongue and Lip Ties
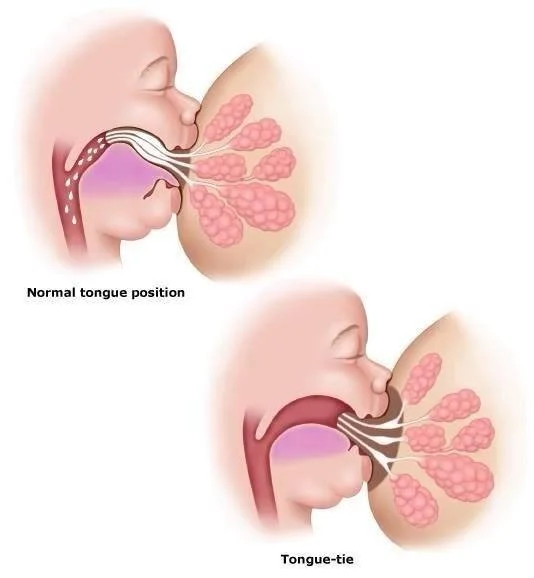
You may have heard the terms "tongue tie" or "lip tie", but what does this actually mean? Simply put, they are congenital conditions where a band of tissue known as the frenulum, or frenum, restricts the movement of the tongue or upper lip. In infants, these ties can affect their ability to breastfeed, causing pain and frustration for both mother and baby. This is how they are most often recognized, so it’s where we will begin:
Breastfeeding issues
For the baby, a tongue or lip tie can limit their ability to latch onto the breast effectively, leading to a shallow latch or painful nursing. This can lead to poor weight gain, frustration, and decreased milk ingestion. Also, infants with ties may experience excessive gas or colic due to swallowing air while feeding. As a result, the baby may not receive adequate nutrition and can become fussy or irritable, affecting their overall growth, development, and, as is often the frustration of new parents: poor sleep.
For the mother, breastfeeding a baby with a tongue or lip tie can be painful and frustrating. The improper latch and inefficient milk transfer can lead to cracked, sore nipples, mastitis, and a decreased milk supply. Mothers may become discouraged and stressed, impacting their overall well-being. Post partum recovery is hard enough without these issues!
Latch Differences
Notice the tongues ability to pull the nipple to the roof of the mouth and latch over the entire areola, versus the shallow latch and lesser milk flow in a tongue tie.
Image from DRGHAHERI.COM, a great resource to learn more.
But wait…
How do you know whether these symptoms are caused by a tongue and lip tie? Often there are actually many factors at play! Birth trauma, tight neck muscles, or fascia issues can also contribute to breastfeeding challenges. That's why seeking the expertise of professionals is so valuable. The first place any mom and baby should go when breastfeeding problems arise is an IBCLC (international board certified lactation consultant) and get their thoughts. An orofacial myologist, physical therapist, chiropractor’s opinion may also be valuable, and we sought all of these in our own journey. (notice- we did not only rely on my training and research as a dentist! A multi-disciplinary perspective is so critical.) These professionals can assess your child's overall orofacial development and help you identify any underlying issues that may be contributing to breastfeeding difficulties. They can also guide you in deciding whether a tongue and lip tie release procedure is necessary for your child.
Here are photos of my son’s ties. There are various ways to grade the severity of these ties- The consensus diagnosis for these would be Class 4 lip tie and Class 3 tongue tie in the other photo.
Other risks involved with tongue and lip ties are less obvious or can show up later in development.
Brain Development
One of the lesser-known but hugely important risks of untreated tongue and lip ties is their potential impact on brain development. The tongue plays a crucial role in the development of the oral and facial muscles, which, in turn influences the development of the cranial bones. If a tongue tie restricts a baby's ability to move their tongue freely, it can lead to altered oral motor patterns. The tongue is directly linked to the brain's sensory and motor regions, making it a critical player in a child's early cognitive development. It plays an indirect role in sleep quality as well.
Sleep Quality
This issue can show up right away in life! As parents, we all know the value of a good night's sleep for both our babies and ourselves. Sleep is crucial for growth and development, and tongue and lip ties can disrupt the harmony of bedtime. Aside from reflux and digestive troubles from poor feeding, tongue ties are highly associated with sleep-disordered breathing patterns in kids and adults. Improper tongue posture can lead to mouth breathing, which is associated with lessened sleep quality. In young children whose brains are developing so rapidly, this can have life-changing consequences. Not only is long term brain development and maturation compromised by poor sleep, but a child’s next-day behavior will be different too. Think of your child when they are tired. They’re probably more irritable, less obedient, more challenging, and despite poor rest are possibly even more energetic than normal. There’s a lot of thought that the poor sleep from mouth breathing has led to an increase in clinical diagnoses like ADHD in kids. I could write a ton more on this topic but am leaving it at that for the sake of (relative) brevity.
The bottom line is that the brain does not grow and develop optimally without proper sleep, and mouth breathing prevents proper sleep.
Respiratory and immune health
As kids grow, the inability to have ideal oral posture will also restrict the tongue’s ability to rest against the palate and naturally push the upper jaw out and forward. Since the upper jaw is the base of the nasal airway, the effect of a baby’s mouth-breathing snowballs into a narrow-palate teenager or adult who is all but forced to be a perpetual mouth breather! (Check out Napolean below!)
Nasal breathing provides a natural filtration system, humidifying and warming air before it reaches the lungs. This natural system is a huge part of our immunity against airborne viruses, bacteria, and other pollutants or allergens. Mouth breathing is also highly associated with sleep apnea in adulthood, which is strongly correlated with a host of other metabolic and psychiatric illnesses.
Attractive Jaw Development
Your child's smile is not just a charming feature but also a reflection of their overall oral and facial development. We’ve seen above that a tongue or lip tie can affect the oral posture of your child, which can lead to a series of esthetic issues. These include misaligned teeth, a narrow palate, and a slack jawed appearance. “Long face syndrome” distinguishes this pattern of growth from a wider, more defined and square jawline. See my friends Napolean and Superman below.
Compare Henry Cavill’s jaw development to Napolean Dynamite. Notice Napoleans longer and more narrow face/jaw structures and open mouth posture. You can note the bags under his eyes and the inattentive gaze. Cavill (Superman!) has a more defined, square jaw. His lips are shut as he nose breathes. Napolean mouth breaths so much he needs some extra chapstick (“But my lips hurt real bad!”)… I wonder if Napolean has a tongue tie!
The impact of these esthetic issues may not be immediately apparent, but they can manifest later in life. By addressing tongue and lip ties early on, you can promote healthy oral development and potentially prevent the need for orthodontic treatment in the future. This potentially saves time, money, and inconvenience for your child later in life during orthodontic treatment, and strongly contributes to a healthy, attractive jawline as an adult.
Speech Development: Untreated tongue and lip ties can impact speech development, because they restrict the movements of the tongue and lips. These conditions may lead to speech articulation problems, making it challenging for children to pronounce certain sounds correctly. The sequelae of restricted communication, reduced confidence, and possibly poorer academic performance “speak” for themselves (pun intended!) Speech language pathologists are a wonderful resource.
Beyond Breastfeeding: Seeking Professional Guidance
In conclusion, it's crucial for discerning parents like you to be aware of the hidden risks of untreated tongue and lip ties. These conditions can affect not only breastfeeding but also brain development, sleep quality, speech, and esthetic jaw development. By consulting with the right professionals you can address the root causes and make informed decisions for the well-being of your little ones.
As my own journey with my son's ties unfolded, we decided we wanted to address the root cause of all these issues, which in his case was the tongue tie and lip tie. But contemplating the frenectomy procedure for our little guy was hard! I’ll talk more about that in the next part of this series and explore the various alternative treatment options.
I’ve got a list of books and resources on this subject if you’d like to learn more! The list below is a good place to start. Please reach out with any questions.
Dr. Brayden Teuscher
P.S. - Our office now offers early intervention airway orthodontics. We are helping kids as young as 3 years old to develop strong jaws with open airways. Check out our Airway Orthodontics info page learn more.
References:
Smith R, et al. (2015) "Tongue-tie: the evidence for division and the significance of professional and parental attitudes." International Journal of Pediatric Otorhinolaryngology.
Geddes DT, et al. (2008) "Frenulotomy for breastfeeding infants with ankyloglossia: effect on milk removal and sucking mechanism as imaged by ultrasound." Pediatrics.
Guillemin M, et al. (2013) "Ankyloglossia as a risk factor for maxillary hypoplasia and temporomandibular joint dysfunction." The Angle Orthodontist.
Lowe A, et al. (2012) "Tongue tie and lip tie: evidence and response." Clinical Lactation.
Martinelli RL, et al. (2016) "Ankyloglossia: The adolescent and adult perspective." International Journal of Pediatric Otorhinolaryngology.
https://www.drghaheri.com/blog
BOOKS BELOW
Walker, M. (2017). Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner.
Moore, S. (2018). Sleep Wrecked Kids: Helping Parents Raise Happy, Healthy Kids, One Sleep at a Time. Grammar Factory
Nestor, J. (2020). Breath: The New Science of a Lost Art. Riverhead Books.
Buchanan, S. (2019). Jaws: The Story of a Hidden Epidemic. Chelsea Green Publishing.
Gelb, M., & Howley, H. (2019). Gasp: Airway Health - The Hidden Path to Wellness. HarperOne.
McKeown, P. (2015). The Oxygen Advantage: The Simple, Scientifically Proven Breathing Techniques for a Healthier, Slimmer, Faster, and Fitter You. William Morrow.
Gum Disease Linked to Severe COVID
The science is clear: gum disease makes COVID worse.
Do your gums bleed when you floss? If your answer is YES, you are not alone. Well over half of US adults have gum disease. Read below to learn more!
Dr Brayden talks about gum disease’s systemic implications
Do your gums bleed when you floss? If your answer is YES, you are not alone. Well over half of US adults have gum disease, and though bleeding is one indicator, it’s likely a majority of people are unaware of their disease.(1) The US surgeon general has called gum disease a “silent epidemic”, and this disease is often ignored despite being highly treatable.(2,3) Because gum disease can affect your overall health and your finances in addition to your mouth, we are reposting this blog series to talk about it. These posts will define what gum disease is, how it interacts with our whole body health, and how it impacts our wallets.
Gum Disease and COVID
We know people who are at “high risk” tend to have the worst COVID symptoms. Many factors can put someone in that “high risk” category, and one of them is gum disease. Several studies have shown that people with gum disease are between three and five times as likely as someone with healthy gums to have severe COVID illness leading to ICU admission or even death. The science is clear: gum disease makes COVID illness worse. Keep reading to find out why!
What exactly is “Gum Disease”?
When we talk about “Gum Disease” we may be referring to two distinct conditions. One is gingivitis, which refers to gum (gingiva) inflammation, or swelling (-itis). When a person has gingivitis, their gums become inflamed, or swollen, with blood and immune system cells. We will discuss the most common reason for this inflammation below. Gingivitis is the first stage of the second even more serious gum disease condition of periodontitis, or periodontal disease.
As opposed to gingivitis, periodontitis refers to inflammation around teeth (perio=around, dont=tooth, itis=inflammation). When inflammation spreads from the tops of gums (gingivitis) to the area surrounding teeth (periodontitis), the classic sign is bone loss, which we measure via radiographs and probing depths. We will discuss the mechanism of bone loss below. 47% of US adults have periodontitis, or periodontal disease, but a large portion of the remaining 53% may have gingivitis, which, without treatment, leads to periodontitis.(1) The scary truth is that gum disease is usually painless and has no symptoms at all during the early stages of gingivitis and mild periodontitis, so it can go unrecognized initially. Unfortunately, the more advanced the gum disease, the greater the systemic health implications – meaning that gum disease can affect other parts of the body and other diseases as well, some of which we discuss below.
How does Gum Disease Progress?
We can almost think of gum disease in two ways: as an infection, and as an inflammatory process.
Gum Disease as An Infection
Gum disease typically will start as gingivitis. The gums become inflamed due to dental plaque- the sticky matrix of bacteria and food debris that gets stuck to our teeth when we don’t clean them well. Eventually, the soft, sticky plaque hardens into calculus, which also harbors bacteria but can only be removed by a dental hygienist. The bacteria and bacterial products induce an immune response from our gums that tries to eliminate what our body is sensing as an infection.
In fact, when our gums are inflamed and bacteria are present in sticky plaques or clinging to calculus, even the simple act of chewing can cause the release of bacteria or their toxins into our bloodstream creating a condition known as bacteremia, or bacteria in the blood. (4)
Usually the increase of bacteria in the blood is transient, or short-lived. But sometimes metastatic infections can occur and become chronic infections, especially if a person has artificial joints or heart valves, atheromas, or is otherwise immunocompromised.(5) In fact, the species of bacteria present in gum disease have been found to specifically predispose us to “systemic diseases such as cardiovascular disease, oral and colorectal cancer, gastrointestinal diseases, respiratory tract infection and pneumonia, adverse pregnancy outcomes, diabetes and insulin resistance, and Alzheimer’s disease”, as reported in Clinical Microbiology Review.(6) Plaque is just the first stage of bacterial colonization.
The worse the gum disease condition, the higher incidence of bacteremia and risk of complications.(7) And, considering there may be up to a trillion dangerous bacteria per diseased tooth, it’s best to nip gum disease in the bud before it develops!
Gum Disease as an Inflammatory Process
Usually we talk about plaque and bacteria causing gum inflammation. But so can pregnancy, certain drugs, and hormonal changes due to puberty or menopause. Inflammation from gingivitis, when untreated, will cause oxidative stress in our bodies, and cytokines to be released from the epithelial lining of our gum pockets. These cytokines are like a messenger system for our body, and they attract immune cells. This process eventually results in the breakdown of our connective tissue and jawbone loss surrounding our teeth. A dental team would be able to see this bone and tissue loss via radiographs and probing depths . Tissue loss around teeth leads to an increased likelihood of tooth mobility (loose teeth) and, eventually, loss of teeth.
Gum Disease Makes You Sicker
But the inflammation doesn’t just stop around your teeth. Many studies have shown an increase in systemic inflammatory markers as a result of gum disease, meaning that inflammation affects far more than your mouth.(8) This is why people with inflamed gums get sicker than people with healthy gums! We talk more about how gum disease affects speficic illnesses in these blogposts: blood pressure and pregnancy, cancer and diabetes, and gum disease is expensive!
The great news about this sinister inflammatory process is it’s been proven that dental treatment for gum disease will reduce systemic inflammation.(8) If you or a loved one have bodily inflammation, consider making dental treatment a part of your wholistic plan to get healthier in 2023!
At Teuscher Dental, our Focus is to Help You Get Healthy and Stay That Way. Let us know how we can help you on your health journey!
References
1) American Academy of Periodontology. “CDC: Half of American Adults Have Periodontal Disease.” CDC: Half of American Adults Have Periodontal Disease | Perio.org, 4 Sept. 2012, www.perio.org/consumer/cdc-study.htm
2) “Surgeon General’s Report on Oral Health in America.” National Institute of Dental and Craniofacial Research, U.S. Department of Health and Human Services, www.nidcr.nih.gov/research/data-statistics/surgeon-general.
3) Benjamin, Regina M. “Oral Health: the Silent Epidemic.” Public Health Reports (Washington, D.C. : 1974), Association of Schools of Public Health, 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2821841/.
4) Geerts, Sabine O, et al. “Systemic Release of Endotoxins Induced by Gentle Mastication: Association with Periodontitis Severity.” Journal of Periodontology, U.S. National Library of Medicine, Jan. 2002, www.ncbi.nlm.nih.gov/pubmed/11846202.
5) Parahitiyawa, N B, et al. “Microbiology of Odontogenic Bacteremia: beyond Endocarditis.” Clinical Microbiology Reviews, American Society for Microbiology (ASM), Jan. 2009, www.ncbi.nlm.nih.gov/pmc/articles/PMC2620633/.
6) Forner, Lone, et al. “Incidence of Bacteremia after Chewing, Tooth Brushing and Scaling in Individuals with Periodontal Inflammation.” Journal of Clinical Periodontology, U.S. National Library of Medicine, June 2006, www.ncbi.nlm.nih.gov/pubmed/16677328.
7) Carrizales-Sepúlveda, Edgar Francisco, et al. “Periodontal Disease, Systemic Inflammation and the Risk of Cardiovascular Disease.” Heart, Lung and Circulation, Elsevier, 2 June 2018, www.sciencedirect.com/science/article/pii/S1443950618305973.
8) D’Aiuto, F, et al. “Periodontitis and Systemic Inflammation: Control of the Local Infection Is Associated with a Reduction in Serum Inflammatory Markers.” Journal of Dental Research, U.S. National Library of Medicine, Feb. 2004, www.ncbi.nlm.nih.gov/pubmed/14742655.
9) Marouf, Nadya, et al. “Association between Periodontitis and Severity of COVID-19 Infection: A Case-Control Study.” Journal of Clinical Periodontology, U.S. National Library of Medicine, Apr. 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8014679/.
10) Larvin, Harriet, et al. “The Impact of Periodontal Disease on Hospital Admission and Mortality during COVID-19 Pandemic.” Frontiers, Frontiers, 1 Jan. 1AD, https://www.frontiersin.org/articles/10.3389/fmed.2020.604980/full.
COVID-19 and Tooth Sensitivity
Unwanted Dental Side Effect of Certain Vitamin…During this pandemic we’re all doing our best to stay well. Staying home, “Social Distancing”, washing hands, not touching faces, getting plenty of sleep and fluids, and eating a healthy diet are the…
Having COVID is no fun. Most of us will use our entire arsenal to get better quickly! We’ve all heard that staying home, “Social Distancing”, washing hands, not touching faces, getting plenty of sleep and fluids, and eating a healthy diet are the standard pieces of advice. And did you know the severity of COVID illness is related to gum health? All these things make sense! One recommendation may have an unwanted side effect though.
Vitamins
During the pandemic and when sick with COVID, some of us also choose to take extra vitamins, including Vitamin C. While Vitamin C is generally considered safe for most people to take, the World Health Organization and the Centers for Disease Control and Prevention, and many other sources indicate that there is no clear evidence that Vitamin C is helpful for prevention or cure of COVID-19. However, there are studies indicating Vitamin C deficiency seems to be correlated with people being more susceptible to infections and pneumonia, and also with having a lowered immune response.
So for those who do choose to take Vitamin C as part of their fight against coronavirus, it may be helpful to know that one little-known but common side effect of taking Vitamin C can be Tooth Sensitivity: a brief sharp pain that often happens when a person eats or drinks something very cold or hot.
Tooth Sensitivity
The causes of sensitive teeth can include a cavity, cracked tooth, broken filling, teeth grinding, gum disease, receding gums, or worn enamel. Another cause of this sensitivity can be acid erosion. Acid erosion happens when the enamel of a tooth is exposed to acidic food or drink, stomach acid, or things such as Vitamin C – particularly if it’s the chewable kind. This acidity can cause the enamel to lose minerals and soften. While this softening can be temporary, if the tooth enamel is repeatedly exposed to acid it will gradually erode to leave the underlying dentin exposed and nerves irritated.
What You Can Do
If your tooth sensitivity becomes constant, painful, or you experience swelling or other additional symptoms, call us to discuss before it becomes worse. If your sensitivity remains mild, and you tend to eat or drink acidic things – or you’re taking Vitamin C – there are options you can try to gain some relief and also help prevent additional enamel erosion and future problems:
Reduce your intake of acidic drinks such as sport drinks, fruit juices, etc., and drink them quickly or use a straw to limit the amount of time the liquid lingers on your teeth. Swish your mouth with water afterward.
If you are chewing Vitamin C, consider switching to a different form of C that doesn’t remain in your mouth so long. Also swish with plain water afterward, or even swish water with a little baking soda mixed in it – and then spit it out.
Avoid acidic foods, drinks and vitamins right before bed or while exercising when you produce less cleansing saliva.
Use a soft-bristled toothbrush, and brush more gently.
Switch to a toothpaste made specifically for sensitive teeth.
Avoid tooth-whitening treatments, which often increase sensitivity.
Talk with us. There’s a possibility your pain may be caused by high spots or teeth grinding. This is far more common than you may think, and we may be able to help alleviate your pain with simple remedies.
Dry Mouth and Tooth Sensitivity
A constant flow of saliva is our natural defense against acid erosion and tooth sensitivity. However, some prescription medications as well as over-the-counter medications such as decongestants can cause dry mouth. Incidentally, dry mouth is also a risk factor for other serious concerns including oral cancer (see our post on oral cancer for more information). Staying hydrated with pure water is a good first step. If dry mouth is a continued issue for you, be sure to let us know. There are helpful products that can bring relief to this dryness, and we’ve found that some products are more effective for our patients than others. Keep in mind that mouth dryness can have serious consequences so it’s not something to simply dismiss!
The Bottom Line
We all want to do everything we possibly can to keep our families and ourselves healthy. But sometimes our efforts to be safe in one area of life can cause problems in other areas, as in the case of chewing Vitamin C. It’s tempting to try the many suggested home remedies we hear or read about on the internet, but these ideas can be unhealthy or even dangerous. The wisest thing to do is to stick with respected sources for information, such as the Mayo Clinic, Johns Hopkins, the World Health Organization, the Centers for Disease Control and Prevention, the Teuscher Legacy Health Blog, and, of course, call your physician and/or call us when you need individualized advice and questions answered. We are always happy to help.
Stay healthy!
P.S.- if you have any questions about this, or are in need of cosmetic dentistry, implant dentistry, or general dentistry in St Charles, Illinois, give us a call or text! We’d love to help!
Gum Disease, Cancer, and Diabetes
If you are reading this, there’s a high chance you have gum disease.1 In previous posts we’ve discussed what gum disease is and how it can affect pregnancy and heart disease. This post will continue that discussion with a focus on cancer and diabetes. Our hope…
If you are reading this, there’s a high chance you have gum disease.1 In previous posts we’ve discussed what gum disease is and how it can affect pregnancy and heart disease. This post will continue that discussion with a focus on cancer and diabetes.
Our hope through these posts is to help you understand how your oral health is a huge part of your overall well-being. Our information is always well researched, as you can see by our references at the bottom. Keep reading, and let us know if you have any questions or comments!
Oral Cancer
Oral cancer is the 8th most common type of cancer in the US, and the majority of head and neck cancer cases are found in the mouth, particularly the sides of your tongue.2 Cancer is one of the many things we screen for at every exam at Teuscher Dental, and part of why regular dental exams are so important and about more than just teeth and gums. Cancerous lesions appearing on the tongue are correlated with gum disease.3 And inflammation in general is thought to contribute to cancer development. Oral cancer has a high incidence of malignancy, and even when successfully treated can require extensive facial reconstructive surgery to recover from, as exampled by oral cancer survivor Gruen Von Behrens’ before and after photos.4
As stated above, inflammation like that of gum disease can contribute to any type of cancer. That, along with pregnancy complications and heart disease, are just a few of the diseases and complications with direct correlation to gum disease. But research also has demonstrated gum disease links to colorectal cancer, gastrointestinal diseases, respiratory diseases, and Alzheimers to name a few. As more research is done it is all too likely the links will become more clear. Gum disease is no joke.
Diabetes
Both Type I and Type II diabetics are more prone to develop periodontal disease, the advanced form of gum disease, than non-diabetics.5,6 This is especially true for children with diabetes, where gum disease progression happens more quickly and is associated with longer duration of diabetes.7 In advanced gum disease, teeth can be lost due to breakdown of surrounding bone and tissue. Snowballing the problem, we know gum disease is associated with low grade inflammation and oxidative stress. These effects are also known to cause lower saliva output, causing dry mouth, increasing risk for dental caries (cavities) and further tooth loss.8 Aside from poor esthetics, tooth loss is is associated with increased likelihood for dysfunctional dentition- that is, teeth that don’t allow for proper nutritional intake.9 This is a particular problem for diabetic patients. It is a vicious cycle.
Don’t have diabetes? Studies have shown that we can actually predict whether a person is more likely to develop diabetes based on their periodontal health.10,11 While a diagnosis of diabetes depends on blood sugar levels, as with all health conditions there is a spectrum of glycemic control. All aspects of our body’s health are interrelated.
Comprehensive research shows dental therapy for gum disease moderately decreases blood glucose levels in diabetics.12 . When we understand the strong correlation and the severity of issues associated with diabetes, it becomes clear that dental treatment for gum disease should be a part of a comprehensive diabetes medical treatment plan.
References
American Academy of Periodontology. “CDC: Half of American Adults Have Periodontal Disease.” CDC: Half of American Adults Have Periodontal Disease | Perio.org, 4 Sept. 2012, www.perio.org/consumer/cdc-study.htm.
“Oral Cancer Facts.” The Oral Cancer Foundation, 28 Feb. 2019, oralcancerfoundation.org/facts/.
Tezal, Mine, et al. “Chronic Periodontitis and the Risk of Tongue Cancer.” Archives of Otolaryngology–Head & Neck Surgery, U.S. National Library of Medicine, May 2007, www.ncbi.nlm.nih.gov/pubmed/17515503.
Henson, Brian J., et al. “Decreased Expression of MiR‐125b and MiR‐100 in Oral Cancer Cells Contributes to Malignancy.” Wiley Online Library, John Wiley & Sons, Ltd, 24 Apr. 2009, onlinelibrary.wiley.com/doi/abs/10.1002/gcc.20666.
Hodge, Penny J, et al. “Periodontitis in Non‐Smoking Type 1 Diabetic Adults: a Cross‐Sectional Study.” Wiley Online Library, John Wiley & Sons, Ltd, 31 Oct. 2011, onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-051X.2011.01791.x.
Haseeb, Muhammad, et al. “Periodontal Disease in Type 2 Diabetes Mellitus.” Journal of the College of Physicians and Surgeons–Pakistan : JCPSP, U.S. National Library of Medicine, Aug. 2012, www.ncbi.nlm.nih.gov/pubmed/22868018.
Al-Khabbaz, Areej K, et al. “Periodontal Health of Children with Type 1 Diabetes Mellitus in Kuwait: a Case-Control Study.” Medical Principles and Practice : International Journal of the Kuwait University, Health Science Centre, S. Karger AG, 2013, www.ncbi.nlm.nih.gov/pmc/articles/PMC5586723/.
Bhattarai, Kashi Raj, et al. “The Imprint of Salivary Secretion in Autoimmune Disorders and Related Pathological Conditions.” Autoimmunity Reviews, U.S. National Library of Medicine, Apr. 2018, www.ncbi.nlm.nih.gov/pubmed/29428807.
Marina Leite Souza, and Karen Glazer Peres. “Association between Metabolic Syndrome and Tooth Loss.” Journal of the American Dental Association, JADA, Dec. 2019, jada.ada.org/article/S0002-8177(19)30522-7/abstract.
Taylor, G W, et al. “Severe Periodontitis and Risk for Poor Glycemic Control in Patients with Non-Insulin-Dependent Diabetes Mellitus.” Journal of Periodontology, U.S. National Library of Medicine, Oct. 1996, www.ncbi.nlm.nih.gov/pubmed/8910827.
Demmer, Ryan T, et al. “Periodontal Status and A1C Change: Longitudinal Results from the Study of Health in Pomerania (SHIP).” Diabetes Care, American Diabetes Association, May 2010, www.ncbi.nlm.nih.gov/pubmed/20185742.
Chee, B., et al. “Effect of Non-Surgical Periodontal Treatment on Glycemic Control of Patients with Diabetes: a Meta-Analysis of Randomized Controlled Trials.” Trials, BioMed Central, 1 Jan. 1970, link.springer.com/article/10.1186/s13063-015-0810-2.
Gum Disease and Your Wallet
Recently we’ve had a few posts about Gum Disease and how it so strongly relates to your overall health. Today we have a quick look at how it affects your wallet! Check it out below and, as always, you can contact us via call, text, or email with any questions…
Recently we’ve had a few posts about Gum Disease and how it so strongly relates to your overall health. Today we have a quick look at how it affects your wallet! Check it out below and, as always, you can contact us via call, text, or email with any questions.
Money
Need a non-health incentive for treating gum disease? How about saving thousands of dollars? The American Journal of Preventative Medicine (a non-dental organization – receiving no benefit from the results!) researched insurance payment data from over 338,000 patients. The research looked at gum disease patients and patients with healthy gums, and compared their yearly medical payments and hospital visits. The results are almost unbelievable!
The study showed annual savings for a pregnant patient who treats their gum disease is over $2,400, for almost 75% savings! And patients who suffered a stroke but treated their gum disease saved almost $6,000 per year! We’ve written about how gum disease relates to these medical conditions in previous posts.
We’ve written before about how gum disease relates to your systemic health. If you aren’t sure, ask your physician whether treating gum disease matters!
The bottom line is that gum disease is no joke, and nothing to take lightly. At Teuscher Legacy Dental, we are focused on partnering with you to improve your overall health and well being. Hopefully this article is educational and can be used as a resource for your pursuit of a healthier lifestyle. If you have any questions, please give us a call or text! If you learned something from the post that your loved ones can benefit from, please share it with them.
Gum Disease, Heart Disease, and Pregnancy
Well over half of US adults have gum disease, and though bleeding is one indicator, it is likely a majority of people don’t know of their disease. It’s a “silent epidemic”, and has significant effects on your systemic health! At Teuscher Dental, Our…
Well over half of US adults have gum disease, and though bleeding is one indicator, it is likely a majority of people don’t know of their disease.1,2 It’s a “silent epidemic”, and has significant effects on your systemic health!3
At Teuscher Dental, Our Mission is To Serve you. That means providing you with the best wholistic care available today, always research based and in pursuit of excellence. This post gives a little information on how gum disease relates to Cardiovascular Disease and Pregnancy. Keep reading to learn more!
Heart Disease:
Cardiovascular (CV) disease, more commonly referred to as heart disease, is the leading cause of death in the US. Hypertension, or high blood pressure, is the biggest risk factor for developing Cardiovascular disease (and your blood pressure is something our office checks at every dental exam). Heart Disease is also highly correlated with gum disease. In fact, a comprehensive study indicated that people with periodontitis are 66% more likely to have a cerebrovascular event like a stroke, and OVER TWO TIMES as likely for those events to be fatal compared with people without gum disease.4
Why does gum disease make cardiovascular disease more dangerous? Research is ongoing, but we know cardiovascular disease can result from increased blood vessel inflammation, which can, in part, be caused by gum disease pathogens.5 Products and toxins from these bacteria also can cause changes in lipid (fat) metabolism, further contributing to CV disease risk.6 When someone already has a form of CV disease, periodontal pathogens preferentially infect atherosclerotic plaques, and studies show that when this infection occurs, multiple species of periodontal pathogens are often present.7,8
Pregnancy
Know anyone who is pregnant? Pregnant patients with gum disease are up to TEN TIMES more likely to have gestation fewer than 28 weeks, that is, a pre-term birth, according to a comprehensive study. The same study suggests that even mild periodontal disease potentially increases pre-term birth risk by over 300%.9 Gum disease also significantly contributes to low-weight births and in-utero infections.10,11 This association and risk is well documented. The good news is that the risk for pre-term and and low weight births is significantly lower for moms who receive dental therapy for gum disease.12 It should be noted that due to hormonal changes, pregnancy gingivitis is normal. But if you are thinking of becoming pregnant, a great way to decrease risk to your baby is to get screened for gum disease beforehand.
We do limit elective dental treatment during pregnancy, but often the risk to the baby (and mom) is actually greater with no treatment, especially if active dental or gum disease is present. If you are interested, the American Pregnancy Association has guidelines for receiving dental treatment during pregnancy. As always, at Teuscher Dental our top priority is your health and that of your growing baby. We will never push you into treatment that is unnecessary or risky. If you have any questions about your dental health during pregnancy, just give us a call!
In our next post we will discuss how gum disease relates to diabetes and oral cancer.
References
1) American Academy of Periodontology. “CDC: Half of American Adults Have Periodontal Disease.” CDC: Half of American Adults Have Periodontal Disease | Perio.org, 4 Sept. 2012, www.perio.org/consumer/cdc-study.htm.
2) “Patients.” ADA Health Policy Institute FAQ – Dental Patients in the U.S., www.ada.org/en/science-research/health-policy-institute/dental-statistics/patients.
3) “Surgeon General’s Report on Oral Health in America.” National Institute of Dental and Craniofacial Research, U.S. Department of Health and Human Services, www.nidcr.nih.gov/research/data-statistics/surgeon-general.
4) Bahekar, Amol Ashok, et al. “The Prevalence and Incidence of Coronary Heart Disease Is Significantly Increased in Periodontitis: a Meta-Analysis.” American Heart Journal, U.S. National Library of Medicine, Nov. 2007, www.ncbi.nlm.nih.gov/pubmed/17967586.
5) Slocum, Connie, et al. “Distinct Lipid A Moieties Contribute to Pathogen-Induced Site-Specific Vascular Inflammation.” PLOS Pathogens, Public Library of Science, journals.plos.org/plospathogens/article?id=10.1371%2Fjournal.ppat.1004215.
6) Hardardottir, I., et al. “Effects of Endotoxin on Lipid Metabolism .” Effects of Endotoxin on Lipid Metabolism , pdfs.semanticscholar.org/a2c1/9025573414d20d3cb2ffbe491493075834ec.pdf.
7) Chiu, B. “Multiple Infections in Carotid Atherosclerotic Plaques.” American Heart Journal, U.S. National Library of Medicine, Nov. 1999, www.ncbi.nlm.nih.gov/pubmed/10539867.
8) Haraszthy, V I, et al. “Identification of Periodontal Pathogens in Atheromatous Plaques.” Journal of Periodontology, U.S. National Library of Medicine, Oct. 2000, www.ncbi.nlm.nih.gov/pubmed/11063387.
9) Offenbacher, S, et al. “Maternal Periodontitis and Prematurity. Part I: Obstetric Outcome of Prematurity and Growth Restriction.” Annals of Periodontology, U.S. National Library of Medicine, Dec. 2001, www.ncbi.nlm.nih.gov/pubmed/11887460.
10) Sánchez, Andrés R, et al. “Maternal Chronic Infection as a Risk Factor in Preterm Low Birth Weight Infants: the Link with Periodontal Infection.” Journal of the International Academy of Periodontology, U.S. National Library of Medicine, July 2004, www.ncbi.nlm.nih.gov/pubmed/15368875.
11) Madianos, P N, et al. “Maternal Periodontitis and Prematurity. Part II: Maternal Infection and Fetal Exposure.” Annals of Periodontology, U.S. National Library of Medicine, Dec. 2001, www.ncbi.nlm.nih.gov/pubmed/11887461.
12) Kim, Arthur J, et al. “Scaling and Root Planing Treatment for Periodontitis to Reduce Preterm Birth and Low Birth Weight: a Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Journal of Periodontology, Centre for Reviews and Dissemination (UK), Dec. 2012, www.ncbi.nlm.nih.gov/pubmed/22376207.
Two Crucial Cold Weather Health Tips to Know Today!
Lots of sane people love winter weather, but I’m not one of them. Give me the hot sun any day. But everything in life gives us an opportunity to learn, and cold weather is no exception. Here are two cold weather essentials you should know: 1. Nose Breathing is best…
Lots of sane people love winter weather, but I’m not one of them. Give me the hot sun any day. But everything in life gives us an opportunity to learn, and cold weather is no exception.
Here are two cold weather essentials you should know:
1. Nose Breathing is best in cold weather – and the rest of the time too.
Studies show that breathing through your nose (as opposed to breathing through your mouth) not only warms the cold winter air, and cleans and humidifies the air – all good for lung health, but nose-breathing may also improve your memory. Memories have 3 main stages of development: encoding, consolidation & retrieval, and according to a recently published Journal of Neuroscience study, nose breathing – but not mouth breathing – enhances all three of these memory stages. For the athlete in all of us, it’s interesting to note that the nasal-pulmonary reflex closes the lungs when the nose closes and opens the lungs when the nose is more open – the Cleveland Clinic says this may be why elite athletes like using nasal strips during exercise. Nose breathing also warms the air before reaching our delicate lungs, humidifies the air for our throat and lungs, and helps clean the air of bacteria, viruses, allergens, pollutants, dust and more before that air reaches your lungs.
2. Pay Attention to the Warning of Cold Sensitivity when it comes to your teeth.
This is no small thing. According to the ADA, causes of sensitive teeth include tooth decay, cracked teeth, worn tooth enamel, worn fillings, and tooth roots that are exposed because of periodontal (gum) disease, gum recession or even from too-aggressive tooth brushing. The Mayo Clinic says that periodontitis, a form of gum disease, can not only cause tooth loss but some research suggests that the bacteria responsible for periodontitis can enter the bloodstream through gum tissue, possibly affecting your heart, lungs, and other parts of the body. Periodontitis may be linked with respiratory disease, rheumatoid arthritis, coronary artery disease or stroke.
If your teeth are sensitive to cold air, it can be vitally important to heed this warning and take action now with your dentist because periodontal disease can be quite serious, and because other causes of cold sensitivity may be way easier to treat when caught early.
So let the cold weather be an opportunity to learn about your health, and a motivation to take positive action! As always, I’d be honored to help you in any way I can.
Your grateful partner in health,
Dr. Mike
Build Your Legacy
Although many people have heard of Weston Price, not everyone realizes he was a dentist. A man ahead of his time, Dr. Price was one of the first to suggest a relationship between nutrition, dental health, and physical health. He studied the nutrition and overall…
Although many people have heard of Weston Price, not everyone realizes he was a dentist. A man ahead of his time, Dr. Price was one of the first to suggest a relationship between nutrition, dental health, and physical health. He studied the nutrition and overall health of a wide range of cultures, taking particular note of the amount of processed foods and sugars consumed by these cultures. His research led him to conclude that the introduction of a “modern Western diet” was associated not only with a decline in the dental and overall health of the people who ate those foods, but in their offspring he also noticed a developmental decline in proper facial bone structure – resulting in overcrowding of teeth.
Taking care of our dental health today not only affects our overall health in ways we may not realize, but, according to Dr. Price’s research, our choices can also affect the overall health, future dental health – possibly including the need for orthodontics – of our children. We have the opportunity to leave a lasting legacy of health through the choices we make. Why not start building that legacy today?