Mold Exposure, Mouth Breathing, and Why Airway Development Matters More Than Cavities
From a Dad and an Airway Dentist…
Myself and my family around the time we discovered the mold in our home
I’m writing this not only as an airway dentist, but much more importantly, as a dad.
My son experienced mold exposure early in life. My wife and I would do anything for our kids! So, like many families, we took the mold exposure seriously:
We identified and extensively remediated the mold source in our home
For over two years, we’ve focused on my son’s gut health and immune support through a pediatric functional medicine practice.
His supplement regiment and food restrictions are exhausting and expensive! But we’ve stayed the course. And yet, he continues to deal with eczema. You may have had a similar experience.
If you’re a parent reading this, you may be wondering:
“We handled the mold—why are symptoms still lingering?”
This article exists because there is often another piece of the puzzle for growing children that goes unaddressed—one that lives in the airway, jaws, and mouth.
Step One: Mold Exposure Must Be Addressed First
When mold exposure is suspected, identifying and dealing with the source is always step one.
This may involve:
Addressing water damage or hidden moisture
Improving indoor air quality
Professional remediation when indicated
No dental, medical, or supplement-based approach can fully work if exposure continues.
Step Two: Immune & Microbiome Support Often Helps
Many families pursue:
Gut and microbiome support
Immune system regulation
Anti-inflammatory nutrition and supplementation
This work—often guided by functional or integrative medicine providers—is incredibly important.
However, even when these steps are taken, many children still struggle.
Why?
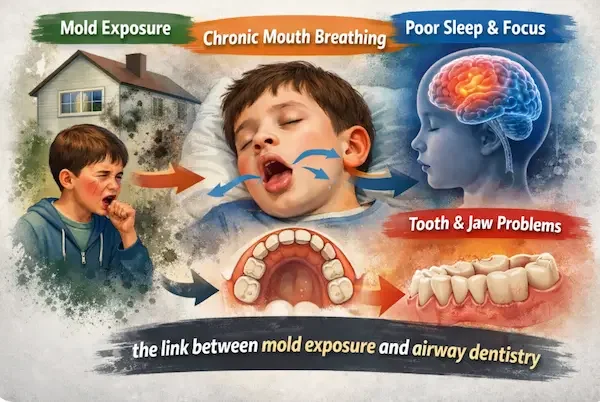
Mold Exposure Often Leads to Mouth Breathing
Mold exposure can cause chronic nasal inflammation, even when allergy testing is negative.
When nasal breathing becomes difficult—especially during sleep—children adapt by:
Opening their mouth at night
Lowering the tongue from the palate
Relying on mouth breathing for oxygen
This is not a bad habit.
It’s a protective response.
But over time, this adaptation can affect jaw growth, airway development, and sleep quality.
Bonus: Another factor that influences mouth breathing can be tongue ties. I wrote extensively about that here.
Why Mouth Breathing Affects Jaw and Airway Growth
Proper facial and airway development depends on:
Even with an extensive supplement list and mold removed, my son still struggles with eczema. Thankfully, he’s still a happy dude!
The tongue resting on the roof of the mouth
Gentle outward pressure that widens the upper jaw
A nasal airway that develops alongside the jaws
With chronic mouth breathing:
The tongue rests low
The upper jaw grows narrow
The palate becomes high and vaulted
The nasal airway becomes smaller
This creates a cycle:
Narrow jaw → restricted airway → worse nasal breathing → more mouth breathing
Long-Term Consequences of Mouth Breathing in Children
1. Jaw & Facial Development (Including Appearance)
Chronic mouth breathing during growth is associated with:
Narrow jaws
Crowded teeth
Recessed or underdeveloped jaws
Longer, less balanced facial growth
This is not about vanity—it’s about structure, airway space, and long-term function.
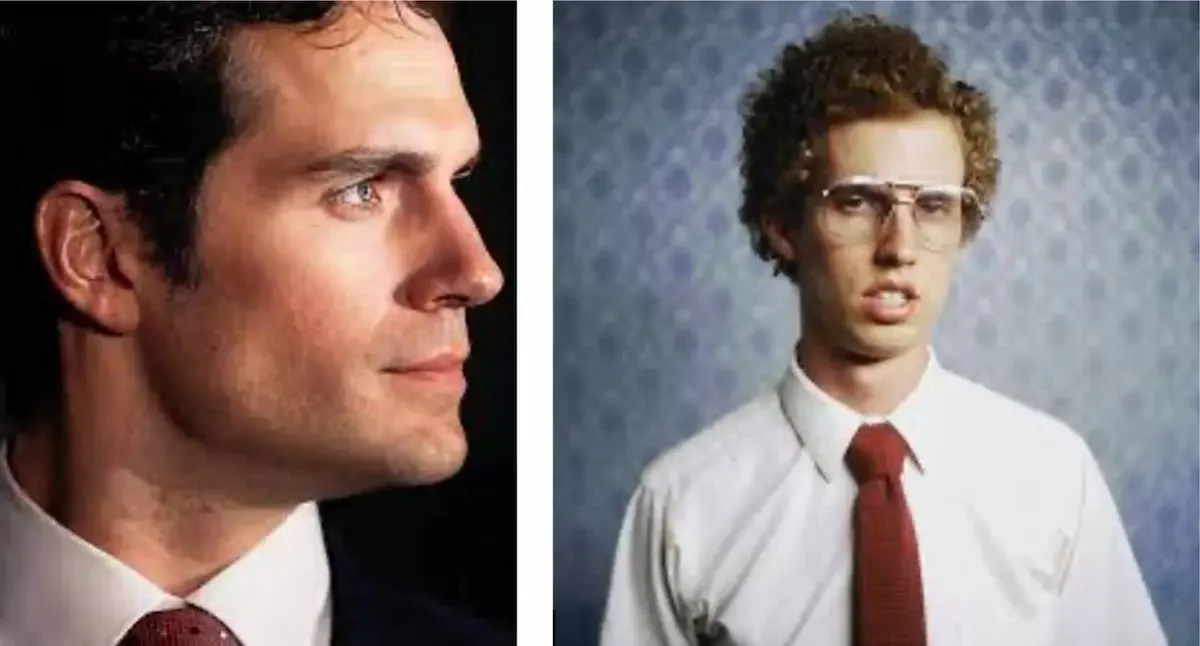
Beauty isn’t necessarily the goal (brain development is. See below.) But it is true that healthy = beautiful. Notice the difference in jaw development in the picture below.
Henry Cavill has a well developed jaw. He is a nose breather! But Napolean Dynamite is notorious for his open mouth and inattention at school!
2. Sleep, Brain Development & Behavior
Healthy brain development requires deep, restorative sleep.
Research shows associations between pediatric sleep-disordered breathing and:
Attention difficulties
Hyperactivity or ADHD-like symptoms
Learning and emotional regulation challenges
Mouth breathing does not cause ADHD—but it can worsen attention and behavior, especially during critical growth periods.
3. Oral Health & the Microbiome
Mouth breathing can also lead to:
Dry mouth at night
Altered oral microbiome balance
Increased cavity risk
Inflamed gums despite good hygiene
Cavities are often a signal of airway dysfunction, not the root problem.
The Key Takeaway for Parents
Cavities matter.
But airway development, jaw growth, and sleep quality matter way more. That’s the perspective of an airway dentist.
Even after mold exposure is addressed and immune support is underway, dental airway evaluation may still be necessary. We always emphasize partnering with functional medicine practitioners and myofunctional therapists!
➡️ In the next post, we explain exactly what an airway dentist evaluates—and what parents can expect…